Our hospitals, emergency departments and ambulatory sites are open to serve the community.
All our facilities are clean, safe and ready for you to get the care you need. To schedule an appointment, please call your doctor’s office. If you need help finding a doctor, call 1-800-MD-MONTE (800-636-6683).
We are happy to welcome visitors to Montefiore and we appreciate your patience, understanding and cooperation.
More details on our increased Visitation Program Guidelines »
Masking is required in the following venues for all staff, visitors, and patients:
-
Critical care areas
-
Oncology units
-
Transplant units
-
Perioperative areas
-
Emergency rooms
-
Around patients with immunocompromising conditions
If you are at high risk for severe illness from COVID-19, you may qualify for antiviral treatments, including oral antiviral treatments. Montefiore Medical Center will be offering prescriptions for Nirmatrelvir/Ritonavir (Paxlovid), Lagevrio (Molnupiravir), or appointments for IV Remdesivir as the most effective treatments against the current Omicron subvariants.
People with COVID-19 have had a wide range of symptoms reported, from mild symptoms to severe illness. Symptoms may appear 2-14 days after exposure to the virus. Individuals experiencing these symptoms or combination of symptoms may have COVID-19:

Cough

Shortness of breath or difficulty breathing
Or at least two of the symptoms below:

Fever

Chills

Repeated shaking with chills

Muscle pain

Headache

Sore throat
New loss of taste or smell
Diarrhea
This list is not all inclusive. Please consult your medical provider for any other symptoms that are severe or concerning to you.
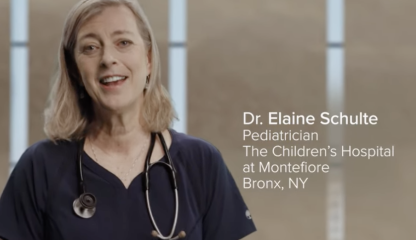
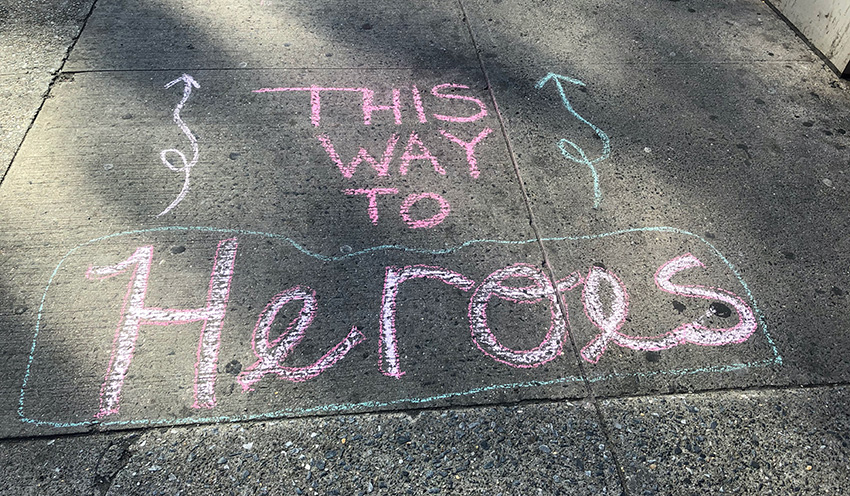
Your Gratitude Keeps Us Going
The current outpouring of appreciation for New York's healthcare workers has been truly humbling. Our community's grace and optimism in the face of hardship inspires us every day. To all those who have cheered and honored our heroes, and to the many who are giving to support our COVID-19 efforts, Montefiore-Einstein would like to thank you. To those who would like to show their support, here's how.
The virus is thought to spread by people in close contact (approximately within 6 feet) through respiratory droplets when an infected person coughs or sneezes. It is also possible to contract the virus by touching an infected surface or item and then touching the nose, eyes or mouth. The virus may be able to live on a surface for a prolonged period of time.